This newborn hyperbilirubinemia assessment calculator is a practical tool for those wanting to quickly assess a child with jaundice – either physiologic neonatal jaundice or pathological jaundice. You will also find out right away if a baby is a candidate for infant jaundice treatment. And, for the curious among you, we will also discuss what causes jaundice in newborns.
Small patients require special care; find out the proper drug amount in the ibuprofen dosage or paracetamol dosage calculator that you should administer when they are in need.
We try our best to make our Omni Calculators as precise and reliable as possible. However, this tool can never replace a professional doctor's assessment.
Why do we measure hyperbilirubinemia in newborn?
You may have noticed that physicians always pay close attention to babies with neonatal jaundice; They assess their physical state often and routinely measure their bilirubin levels. The reason for this is to detect any dangerously high levels of bilirubin before they do any damage. The main concern is kernicterus – bilirubin-induced damage to the brain and central nervous system that can be life-threatening. It is caused by excessive hyperbilirubinemia in newborns. The concentrated bilirubin can then cross the brain-blood barrier, where it is neurotoxic.
However, this condition can almost always be prevented. That's why it's crucial to monitor the baby's bilirubin levels.
How to use newborn hyperbilirubinemia assessment calculator?
-
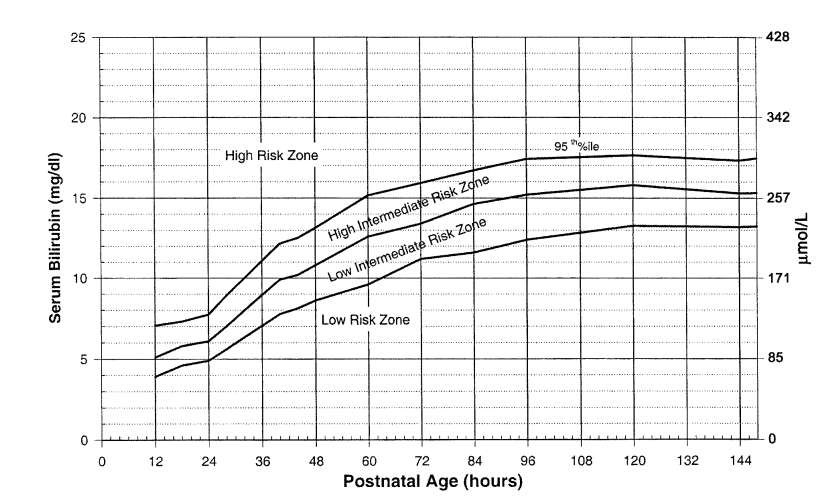
If your child has neonatal jaundice, check if their bilirubin level is within the normal range for their age. First, put in the baby's age – you can choose between hours and days.
-
Then, fill in the bilirubin level field. You can switch between the most convenient units. If the bilirubin was checked, for example, two days ago, remember to adjust the child's age for the moment of the test. This is the only way to make sure the result you'll get is accurate.
-
Check if the baby was born full-term or premature.
-
Check if some of the additional risk factors are present in your baby.
-
The result is ready right away. You can see the range that the baby is in, if there's a risk of bilirubin growing dangerously high, and if there are any indications that you should start an infant jaundice treatment.
The bilirubin ranges used in this calculator are based on the , a source supported by the .
What is jaundice?
Jaundice causes yellow discoloration of the skin, mucosa, and sclera (the white part of the eye).
To understand the roots of jaundice, we have to follow the life cycle of erythrocytes (red blood cells). These are the hemoglobin-filled bodies responsible for carrying oxygen, and they have a lifespan of around 100 days. After fulfilling their function, they must be removed from the body, and the hemoglobin (red pigment) must be broken down. The process of destroying hemoglobin takes place in the liver, where it is first converted to bilirubin (a yellow pigment). Bilirubin is then excreted with bile from the liver into the intestines, where it forms part of the stool. Here it undergoes further breakdown, becoming brown as the iron in the hemoglobin oxidizes. However, such a complex metabolic pathway leaves a lot of room for things to go wrong.
The yellow tint of the skin and eyes reflects the buildup of bilirubin in the body's tissues. This has many different causes, including liver insufficiency, increased blood breakdown (hemolysis), or mechanical obstruction of the bile duct.
What is physiologic neonatal jaundice?
What may sound surprising is that infant jaundice is a normal phenomenon – we call it physiologic jaundice. It arises due to a few things:
-
When in the womb, the amount of red blood cells is significantly greater than after being born – so the little body gets rid of them.
-
Fetal hemoglobin differs from normal hemoglobin. After birth, this hemoglobin is replaced with the regular kind.
-
The infant liver is not yet mature and can't deal with large amounts of bilirubin in a short time.
The result of all those processes is hyperbilirubinemia and – in some cases – neonatal jaundice.
Physiologic jaundice starts on the 2nd - 3rd day of life (not earlier than at the 36th hour of life) and clears up before the child is 10 days old. In prematurely born babies, it usually starts a little later and lasts up until they are 14 days old. The bilirubin levels should never exceed the upper normal limit for the child's age.
Physiologic jaundice clears on its own and doesn't require treatment.
What causes jaundice in newborns?
When it comes to causes of hyperbilirubinemia and newborn jaundice, there are two options – it's either physiologic or pathologic jaundice.
Physiologic jaundice | Pathologic jaundice | |
|---|---|---|
Starts | On the 2nd-3rd day of life (not earlier than the 36th hour of life). | On the 1st or after the 10th-14th day of life. |
Lasts | Up to 10 days (14 in premature babies). | Longer than the 10th-14th day of life. |
Bilirubin levels | Never exceed the upper normal limit for their age. | Are higher than the upper normal limit for their age. |
Urine and stool | They look normal. | The stool is whitish and/or the urine is dark. |
The causes of physiologic jaundice are... well, as the name says, physiologic, so within normal limits. On the other hand, with pathological jaundice, it is always recommended to examine the child carefully and run laboratory tests. The causes of pathologic newborn jaundice include:
- Blood type incompatibility;
- Rh factor disease;
- Biliary atresia;
- Metabolic disorders – e.g., enzyme deficiency or hypothyroidism;
- An infection – e.g., common urinary tract infection.
There is also the curious case of breast milk jaundice. It occurs in newborns who are regularly breastfed, and the yellowish skin color can last up to even three months. Sometimes it is considered to be prolonged physiologic jaundice. The mechanism of the condition is not well-explained. It is usually harmless, as the baby's body learns with time how to break down the excessive bilirubin. The most common action is to monitor the bilirubin level at home.
Infant jaundice treatment
There are two main ways of treating hyperbilirubinemia in newborns:
Phototherapy – the child is placed under special lamps or on a phototherapy mattress with fibreoptic cables, which emit a special type of light. The most common type of light used is blue light (420-560 nm in wavelength). The light promotes chemical changes in bilirubin so that it dissolves in water and becomes easy to remove from the body.
The child's eyes are covered for protection. The phototherapy session lasts for about 24-36 hours, with short breaks for feeding and nappy changing.
Exchange transfusion – as a more severe treatment, it is usually preceded by phototherapy, checking if the baby responds at all to the light. If the response is not large enough, the decision to start exchanging a transfusion is made (check how pediatricians decide on the pediatric blood transfusion volume). During this process, the baby's blood – full of bilirubin – is replaced with blood from a matching donor. As a result, the bilirubin level drops.
🔎 Find out, how much blood there is in your baby's body in the pediatric blood volume calculator.
However, if hyperbilirubinemia has an underlying condition, like infection, causal treatment is necessary.
There is also a particular case of pathologic neonatal jaundice requiring special treatment. It's a rhesus (Rh) factor disease, and the treatment is intravenous immunoglobulin (IVIG). In this case, in the baby's bloodstream, there are anti-Rh antibodies (coming from the mother as a result of a Rhesus incompatibility), destroying red blood cells. IVIG blocks the Rh-antibodies so that they don't attack blood cells anymore.